With countries across the world responding to the threat of coronavirus outbreaks, here in Massachusetts and, more locally, in the Pioneer Valley, local hospitals and municipalities are working to prepare and plan for a potential outbreak of the new respiratory viral strain for which there is currently no vaccine or antiviral treatment.
The coronavirus (also known as COVID-19, a short-hand version of “coronavirus disease 2019”) is spread from person to person and through contact with surfaces or objects, according to the Center for Disease Control’s (CDC) website. Symptoms include a fever, coughing, and shortness of breath, but sometimes they won’t appear until two to 14 days after a person is infected.
Dr. Estevan Garcia, Cooley Dickinson’s chief medical officer, said the risk is low for the Pioneer Valley and Massachusetts to experience an outbreak of coronavirus. But the medical community in the Valley does take the coronavirus risk seriously and has been making preparations.
“A multidisciplinary team is collaborating to ensure Cooley Dickinson is ready to respond, if there is a need to test or provide care for patients with possible COVID-19. At Cooley Dickinson, there are airborne isolation rooms throughout all inpatient units. We have the capacity to increase the number of airborne isolation rooms on individual units and we can also make an entire unit negative,” he said.
In the event of an outbreak of COVID-19, patients who have the virus would be located in a separate part of the hospital from other patients who don’t have the virus, he explained.
“In situations where we could see a surge of patients it’s important to reserve hospital resources for those patients requiring hospitalization while working with community providers and resources to screen patients that are appropriate for home isolation and outpatient supportive care,” he added. “The vast majority of COVID-19 patients will do very well at home with supportive care limiting exposure to others in the community.”
Dr. Sarah Haessler, an infectious disease specialist at Baystate Medical Center in Springfield, said Baystate Medical Group is also actively preparing for coronavirus cases in western Massachusetts.
“We have put into place protocols for our front doors — emergency departments, urgent care centers — for the screening of patients as they come in through the front door to assess them for risk factors for having that COVID-19,” she explained. “We have been screening at the door for over a month now. Ever since the first case appeared in the United States, we’ve been screening.”
Although there isn’t widespread transmission of the virus across the United States, the CDC is advising health care institutions to prepare for an outbreak, she added.
“We should all prepare for the fact that that might come to pass in the U.S.,” Haessler said. “If it doesn’t, that would be great — and wouldn’t it be nice if we overprepared and never had the problem? Fortune favors the prepared, and so health systems need to be ready to do that. I feel really confident that Baystate Health is ready to do that.”
Haessler declined to comment on whether there have been any suspected cases of coronavirus at Baystate Medical Group due to the Health Insurance Portability & Accountability Act (HIPAA) confidentiality requirement.
No treatment yet
The coronavirus isn’t new, but COVID-19 is a novel strain of the human coronavirus family with others including the Middle East Respiratory Syndrome (MERS-CoV) and Severe Acute Respiratory Syndrome (SARS-CoV). The virus that causes the COVID-19 disease is called SARS-CoV-2.
Garcia said COVID-19 will run its course seasonally in the next few months, but the virus will likely return in subsequent seasons, Garcia said.
Antiviral drugs such as oseltamivir phosphate (available under the trade name Tamiflu) are used to treat influenza, which is a viral infection as is COVID-19. However, Garcia explained that antiviral medications don’t work for treating the coronavirus.
“The real concerns are the fact that we don’t have treatment, so the antivirals don’t work at this point, and we don’t have a vaccine,” he explained. “In reality, while they will be starting some testing for a phase one trial, it will be over a year for a vaccine to work in a large way — to start vaccinating communities.”
The vast majority of people infected with COVID-19 will recover, Garcia said, but the concern is that the mortality rate for the virus is up to 20 times higher than the seasonal flu (influenza). During the past 10 years, the mortality rate in the United States from the flu was just 0.1 percent.
During the 2018 to 2019 influenza season, an estimated 34,157 people died of the flu in the United States, according to data from the Center for Disease Control.
According to the World Health Organization, the mortality rate for coronavirus patients in Wuhan, China, the city where the virus emerged, ranges from 2 to 4 percent, but the mortality rate for the rest of China is 0.7 percent.
“The folks that it appears are being affected most severely by disease are the elderly and young infants and children, which tends to happen with current influenza,” Garcia noted. “That’s the group we’re most worried about. If we do have an outbreak of this, there will be lots of upper respiratory infection, and it will be easily transmitted because of the cough and sneezing. The concern is that you’ll get large groups of people — entire schools or classrooms that are infected and need support.”
As for helping to curb the spread of the virus, Haessler said one of the most important methods is for people to wash their hands with soap and water or cleanse them with alcohol-based hand sanitizers.
Garcia said because the coronavirus is immune to antiviral medication, one of the best methods to prevent the spread of the virus is by canceling events with large groups of people, working from home, and using other social distancing methods.
“In these situations, it’s really important for patients who are concerned not to flood the health care facilities because if you’re concerned and you’re not ill, then it can become overwhelming to take care of patients that are ill. Everything that we take care of every day, besides COVID-19, we will still be taking care of every day.”
Forget the face masks
Although face masks are selling out throughout the country, U.S. Surgeon General Jerome Adams advised that members of the general public stop buying masks in a tweet on Feb. 29, writing, “They are NOT effective in preventing the general public from catching coronavirus, but if health care providers can’t get them to care for sick patients, it puts them and our communities at risk!”
Haessler said the face masks are designed to prevent spreading infections.
“The type of mask that health care workers wear in the hospital, to care for people with respiratory pathogens to prevent them from getting that, is a different type of mask that isn’t available widely to the general public,” she explained. “The reason for people in the public to wear a mask is if you, yourself, are symptomatic with an infection and are trying to prevent the spread to other people.”
Garcia said he recently spoke with officials with the Massachusetts Department of Public Health over the phone, and they told him that there are airports that have health care screening facilities to determine if people were on international flights in countries where coronavirus outbreaks have occurred and whether they’re showing symptoms.
“From there, they’ll have their screening to determine whether or not they need to go to a health care facility. If they don’t, they are allowed to travel home and are asked to self-monitor for those 14 days for fever and development of systems,” he said.
However, one of the biggest challenges for the state is testing people for the coronavirus, Garcia noted.
“The CDC is really who tests for COVID-19,” he said. “We receive specimens here, send the specimens to the state lab, who then coordinate with the CDC. Our state lab is still not able to test for COVID-19, and there are really only 12 municipalities outside the CDC labs that are able to do the testing.”
The U.S. Food and Drug Administration gave approval of the Massachusetts State Public Health Laboratory to begin testing patients for COVID-19, the state health department announced on Feb. 28.
“If someone is ill and we send the test, it’s going to take time to come back and then that patient is going to have to stay in isolation,” Garcia added. “Because there’s so many steps with this, it’s several days. As soon as the state, hopefully within the next few days or weeks, is able to do the testing, then that will reduce the time.”
There has only been one confirmed case of coronavirus so far, according to the most recent data available from the state’s health department. There have been 608 people in the state who have been monitored or are undergoing monitoring for COVID-19: 377 of those people already completed monitoring and have been released after not showing symptoms, while 231 are still being monitored and are currently in self-quarantine.
Updated information will be posted to the Mass DPH website on Wednesday and will continue on a weekly basis, according to a DPH representative.
“We understand the concern this new virus is causing and want to reassure residents that at this time there is still a single confirmed case of COVID-19 in the Commonwealth and the risk in Massachusetts remains low,” Mass DPH Commissioner Monica Bharel wrote in a statement.
According to another statement by DPH, the department is instituting a streamlined organizational system for an outbreak called an incident command structure, which would include briefings with state health leadership regarding responses to a potential outbreak. DPH is also working to keep local public health institutions, boards of health, school health personnel, emergency medical services, college and university health systems, and health emergency preparedness teams informed about the coronavirus.
‘The first line of response’
For now, municipalities across the Pioneer Valley are taking precautions amid growing concerns over the coronavirus.
Easthampton Mayor Nicole LaChapelle has huddled with the city’s health agent, Bri Eichstaedt, and chiefs of the fire and police departments about emergency health plans should the threat level rise to pandemic, although she wants to make sure “not to dramatize the issue, but provide cold, specific, hard facts.”
The city’s various departments are preparing for a possible public safety emergency in coordination with the Massachusetts Emergency Management Agency — the agency that coordinates federal, state, local and private resources throughout the commonwealth during times of disasters and emergencies — according to LaChapelle.
Transporting infected people to local medical facilities during an outbreak is just one response the city would coordinate, LaChapelle said. Public buildings and spaces, such as City Hall and the Council of Aging, could also close temporarily in an emergency. Additionally, the mayor’s administration would have to determine what public services would need to be paused should that become necessary.
“The first line of response — public health, fire, and police — are so well trained to respond as needed,” LaChapelle said.
At the moment, the city’s health and public safety departments are coordinating with state agencies to monitor reports of the coronavirus in the state and what responses, if any, are needed should the situation change.
“We are getting information out there, watching as things change, and putting information out as soon as possible,” LaChapelle said.
Northampton Director of Public Health Merridith O’Leary said the city is coordinating with the Hampshire Public Health Preparedness Coalition, which for the past 18 years has served as the county’s response coalition for potential health emergencies.
She explained that the coalition brings together a team of department leaders — working in schools, hospitals, utilities, and emergency services — who focus on providing local residents with communication about the virus and planning for a potential outbreak.
Northampton Assistant Fire Chief Jon Davine, who also serves as the city’s emergency management coordinator, said this week city officials will be meeting with representatives from local public schools, the board of health, the Hampshire Public Health Preparedness Coalition and Smith College to develop an action plan if a coronavirus outbreak were to occur in Northampton.
O’Leary said one potential idea that could be implemented after the meeting would be to have doctors take house calls to help prevent the spread of the virus.
“We don’t want people who are asymptomatic to travel,” she explained.
Right now, the coalition isn’t considering creating an emergency dispensing site in the event of an outbreak because there’s no vaccine for the new strain of the virus, O’Leary noted.
Currently, Northampton’s dispatchers ask residents calling emergency services if they’ve recently traveled to another country. If callers have traveled abroad recently, emergency medical responders are informed and take precautions to limit exposure. From there, Cooley Dickinson Hospital is alerted to a suspected coronavirus case.
Preparing at home
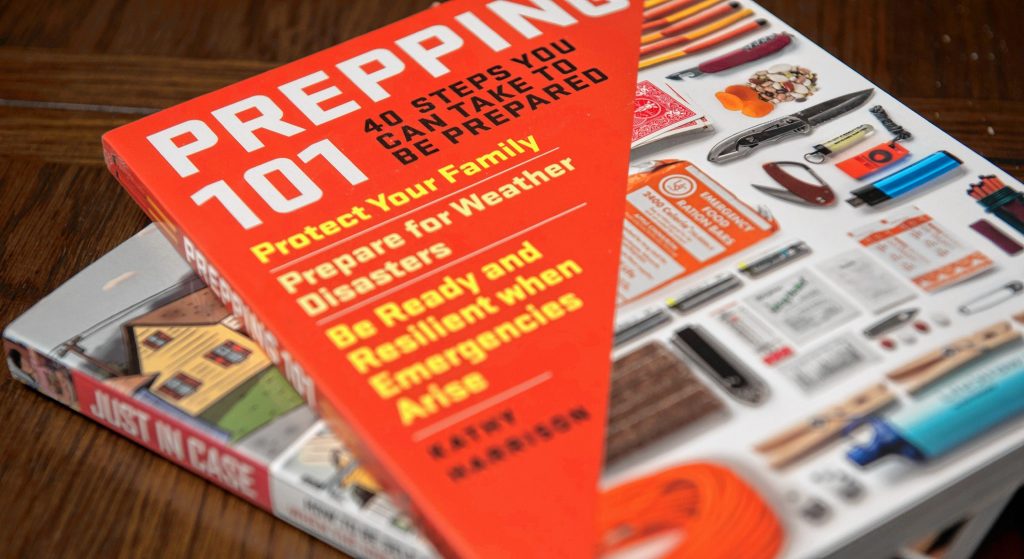
Kathy Harrison is a 68-year-old Easthampton resident and published author who writes books about preparing for disasters. Her works include the 2018 book Prepping 101: Forty Steps you Can Take to be Prepared and the 2008 guide Just In Case: How to Be Self-Sufficient When The Unexpected Happens.

Kathy Harrison, author of “Prepping 101” and “Just in Case,” talks about the best way to prepare for the possibility of the coronavirus becoming a pandemic.
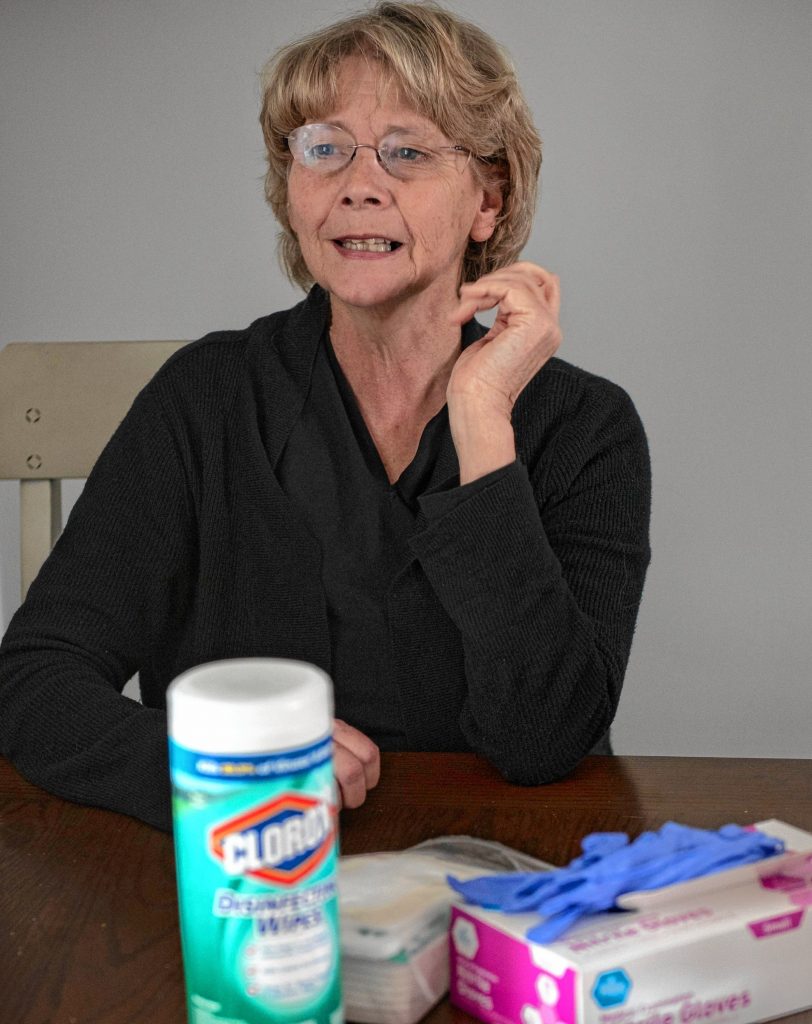
In her apartment last week, Harrison placed a week’s worth of food supplies on her kitchen table, including oatmeal, canned tomatoes, and pasta, as well as other shelf-stable food, showing what she and her family would eat if an outbreak of the coronavirus hit the Pioneer Valley.
“We could manage for maybe three months,” she said, noting that in addition to nonperishable food items, she also stocked up on personal hygiene products and disposable gloves, which she’d wear while going to the supermarket to help prevent catching the virus.
For other disasters such as hurricanes, tornadoes, and winter storms, Harrison said communities are more prepared for when the electricity goes out. But for a viral outbreak, people have to prepare for isolating themselves.

Kathy Harrison, author of “Prepping 101” and “Just in Case,” displays a range of grocery items she has stocked up in case of emergency. In the case of coronavirus, Harrison says people should have nonperishable food items on hand in case there is the possibility of a quarantine.
“We’re not prepared for having to stay home for a month,” she added. “That is hard to do.”
She thinks preparing for disasters ahead of time is a civic responsibility to make sure critical resources aren’t taken away from people who need it the most.
Harrison also worries that the United States is unprepared for an outbreak of a coronavirus and that if a vaccine is developed for COVID-19, low-income households won’t be able to afford it.
Access to excellent medical care can make a big difference, she added, and the way people interact with their neighbors should be just as important as federal and state responses.
“Concentrate on your family, then concentrate on your neighbor — your wider community… if you have senior citizens and single moms living near you. And then your community and your town,” she said. “That’s your best effort at containment and education.”
Chris Goudreau can be reached at cgoudreau@valleyadvocate.com. Staff Writer Luis Fieldman also contributed to this story.