Dino Schnelle, a 66-year-old resident of Heath, was diagnosed with Human Immunodeficiency Virus (HIV) in 1996. An openly gay man, he contracted HIV through unprotected sex sometime in the early- to mid-1980s.
He waited about a decade before getting tested due to fear of dying from HIV, and has kept the virus under control with drugs that, while covered by insurance, are extremely expensive.
But recently, the medical community reported that two patients have been determined to be cured of HIV, increasing hope that scientists can find a full-blown cure for the disease. Schnelle, said if a cure for HIV were to be found, he’d be willing to try it.
“The side effects from the early pills were horrible side effects and I was willing to tolerate them because we were kind of like human guinea pigs at that point … The FDA was taking 10 years to approve HIV drugs and people were dying by the thousands because there were no treatments. All of us stood up and said, ‘Experiment on us.’ I’d be willing to do that again.”
At the same time, the realities of health care in the United States and the history of how patients with HIV and AIDS have been treated over the decades make him skeptical that such a cure would be financially accessible to the vast majority of people who suffer from HIV.
The three-drug combination Schnelle now uses to suppress his HIV costs about $4,000 month. He argued that more than 20 years after HIV drugs being available to patients they shouldn’t be as expensive as they are today.
“Why is it after 20 years that these drugs are so expensive in the United States when they’re life saving, while in Africa they’re able to produce them for cents on the dollar?” he asked. “The big decrease in death rate of HIV and AIDS in Africa is because they are able to come up with low cost HIV drugs. Why can’t we do that here?”
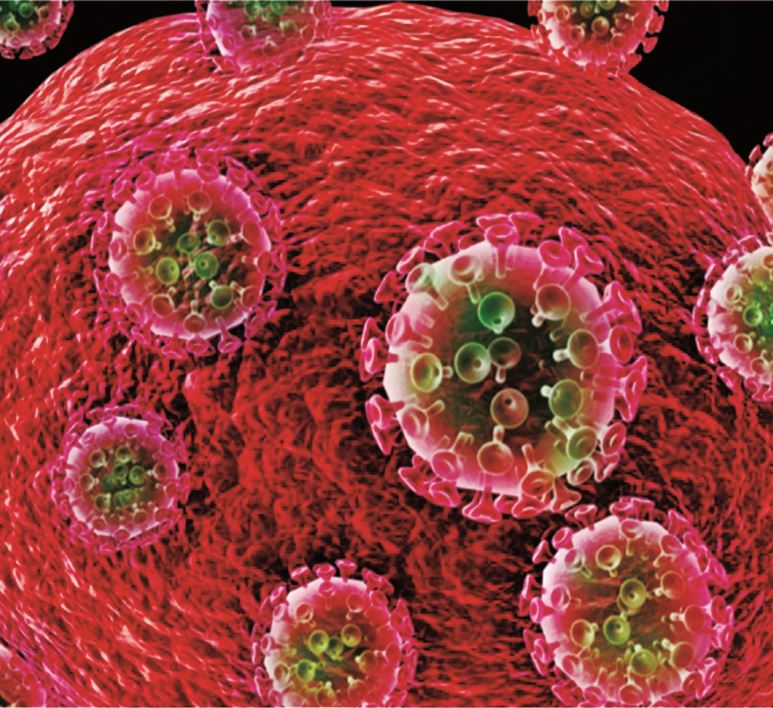
Throughout the 1980s and ‘90s, hundreds of thousands of people with HIV contracted Acquired Immune Deficiency Syndrome (AIDS) and died as a result of their illness. AIDS was a death sentence. There was initially no treatment for HIV before it turned into life threatening AIDS and it took years before the first HIV antiretroviral drug was approved by the FDA.
Today, those with HIV have medication to keep the disease under control, but a cure or vaccine for the disease has thus far eluded researchers.
Now, with a potential cure on the horizon, those with HIV and local HIV support organization leaders are emphasizing that in addition to a cure, equitable economic access to treatment would be just as vital to ending the disease. Right now, a small majority of people living with HIV aren’t in regular treatment and progress to prevent HIV has stalled in recent years.
In Massachusetts, there’s also been a rise in HIV infections due to the ongoing opioid crisis, which adds to the problem of controlling the HIV epidemic.
Meanwhile, President Donald Trump announced earlier this year in his State of the Union address that the United States would seek to eliminate HIV/AIDS by 2030, but the amount of funding allocated to reach that goal isn’t enough and many remain skeptical.
Schnelle said he probably lived with the virus for a decade before getting a diagnosis during which time six friends contracted the disease and died of AIDS. After his brother died of AIDS in 1996, he decided to seek treatment.
“It wasn’t until my youngest brother [Ken] was diagnosed with full blown AIDS and died the summer of 1996 that I went and got tested myself,” he said. “Because at that point, AZT had come out, which was the first antiretroviral drug.”
It’s been more than 20 years since Schnelle was diagnosed and began receiving treatment for his HIV.
“Becoming HIV positive became a lens that I looked at my life through,” he explained. “A lot of things became extremely clear as to what was important to me about family and friends and the relationships I have with people; living every day to the fullest.”
Schnelle said he’s more worried about a list of other ailments that he has to deal with every day such as bad joints, having a heart attack, high cholesterol or diabetes compared with his HIV.
“It has gotten to the point where the only time I really think about it is when I’m taking my pills,” he explained, adding that at one time he was taking 18 to 20 different pills a day for three different medications and often had to wake up at 2 a.m. to take his pills. Today, he takes four pills twice a day.
For Schnelle, the side effects of taking HIV drugs have included constant nerve pain in his limbs and having his body fat redistributed to his gut, a common side effect for some HIV treatments.
But it can also be difficult to determine whether some of his symptoms are due to the virus itself or the treatments. One of the long term effects of the virus is also nerve pain and damage, which for Schnelle, is more intense because he went undiagnosed for 10 to 12 years, he said.
There are now two patients who’ve been essentially cured of HIV, but only because of life-threatening bone marrow transplants, which were used to treat their cancer. But this new medical breakthrough is giving some hope for a more practical cure in the future.
A man known as “the London patient,” who was diagnosed with HIV in 2003, was diagnosed with stage four Hodgkin’s lymphoma in 2013. He underwent a bone marrow treatment intended to treat his cancer, which resulted in being essentially cured of his HIV, though scientists say he is in long-term remission.
Another case with a patient, Timothy Ray Brown, known as “the Berlin patient,” was 12 years prior, according to information from “Lessons Learned from a Second HIV ‘Cure’” case by Brian Wood, a medical doctor with the Infectious Diseases Society of America. Brown also had a bone marrow transplant to treat his cancer.
But what does this medical breakthrough mean for people living in the Pioneer Valley who are HIV positive? Not much … yet, according to Dr. Eric Granowitz, an infectious disease specialist with Cooley Dickinson Hospital in Northampton, who has been seeing HIV infected patients since the 1980s, Schnelle among them.
“When they gave [the London Patient] stem cells from another person, they gave him back stem cells from a person who was resistant to HIV,” Granowitz said, describing the case. “It’s a certain genetic mutation. Now it doesn’t appear that he has HIV anymore. The HIV was eliminated from his body.”
Granowitz said this potential HIV cure isn’t an option for every person who is HIV positive because the bone marrow transplants are life threatening procedures and ultimately impractical.
“What’s exciting about the second patient is that he showed that the first patient wasn’t a fluke,” he explained. “It’s kind of re-proof of process. It’s very exciting to hear because it gives researchers something to look at. Maybe we’ll have cures down the line? We obviously don’t want people to take medications if they don’t need to. It would be better to cure them. Ideally, it would best to have a vaccine to prevent it in the first place, but that’s proven very difficult.”
HIV can affect anyone, but both historically and currently, it has largely affected marginalized groups.
Gay and bisexual men make up the greatest at risk group with an estimated 26,000 average of new HIV infections per year in the United States, according to the Center for Disease Control and Prevention (CDC). In 2016 the CDC estimated that nearly two-thirds of the approximately 38,700 Americans who were newly infected with HIV were gay and bisexual men.
Following a decline between the years 2008 and 2014, instances of new HIV cases have increased, according to the CDC.
The CDC estimates that the rate of HIV infections has bounced back, in part, because HIV prevention and treatment are not reaching communities that could benefit from among black and Latino communities, which are disproportionately impacted compared to white communities.
Overall, there are approximately 1.2 million people in the country living with HIV today and about 14 to 15 percent of those people haven’t been diagnosed, according to HIV.gov.
Betsy Shally-Jensen, director of A Positive Place in Northampton, a resource program for those who are HIV positive in the Valley, said it’s more than just a funding issue when it comes to HIV/ AIDS.
She argued that racist policies create disparities for those who are HIV positive among black and Latinx communities. She said that homophobia, transphobia, and the stigma around poverty all contribute to the problem.
In 2016, the CDC estimates that 9,800 people newly infected people with HIV were black gay and bisexual men, while 8,300 were gay and bisexual Latino men, which were the first and second highest groups of people for that year. The third highest population was white gay and bisexual men, which accounted for about 6,700 people.
In western Massachusetts, HIV has risen among young gay Latino men, she said. Transgender women are also statistically at a higher risk on average.
“It’s not just a medical cure that we’ve been looking for,” she said. “It’s all the spokes in the wheel that make this thing called HIV. It’s about dignity and respect and equity because who’s at the highest risk? Who carries the highest burden? If it was just about medicine and taking a pill there would be no disparities in the populations.”
Shally-Jensen said the medical community needs to start asking patients about their sexual histories, drug use, and living conditions, in order to help curb the spread of the disease.
“You can have a cure out there, but the disease is still going to be spread if people aren’t talking about how transmission occurs with patients,” she said.
A cure for HIV would only work if issues such as social determinants of health and systemic inequities are addressed too, Shally-Jensen said.
“When there’s a perfect storm of all of that coming together, then we’ll see an end,” she said.
Shally-Jensen thinks that stigma is still a problem for HIV/ AIDS patients. Often clients at A Positive Place still enter through the back door.
Shally-Jensen said she still hears stories about clinical providers wearing full protective gowns and masks when they see someone who has HIV or AIDS. It’s not a common occurrence, but it still happens.
“Stigma is one thing that’s run through the epidemic and one of the most important things that we can do is value each and every person who comes through the door and make sure that they know that,” she said.
Shally-Jensen said whereas other local HIV/AIDS support organizations such as Baystate Health and Tapestry focus on prevention, A Positive Place, which is a program of Cooley Dickinson Medical Group, has provided free services to HIV positive patients since 1991.
“What do we do? We make sure that folks are linked to medical care. We have very close relationships and we partner with the infectious disease doctors in the area. In Massachusetts, the way that we provide HIV healthcare is through infectious disease specialists … Most people have a primary care physician and an [infectious disease doctor.]”
She said A Positive Place works to engage with clients to make sure they have everything they need as they undergo HIV treatment.
“The people who are HIV positive who have a job, who have a social support network, and a place to live, don’t come here for support … Most of our clients are on MassHealth, so that shows you the income level of folks who come here.”
A Positive Place also has its own grant-funded housing program with about 25 subsidies for people who are HIV positive and chronically homeless.
Shally-Jensen said there’s no doubt in her mind that opioid use has contributed to the rise of HIV cases in Massachusetts.
“There’s certainly a rise because of the opioid crisis,” she said. “I think that’s probably the major reason why we see a rise.”
State data backs up that claim.
Gay and bisexual men have has always accounted for the largest population impacted by HIV, but the second are those who use intravenous drugs … and those numbers are rising.
“Increases in HIV infection among people who inject drugs is a consequence of the current opioid drug use epidemic,” states 2017 state report.
The number of individuals living with HIV in Massachusetts has increased by 23 percent from 2007 to 2016, according to a state report, which named the opioid drug epidemic as one of the causes.
State researchers found that Springfield is ranked third in Massachusetts — after Provincetown and Boston — for having the highest rate of HIV infections with about 806 cases per 100,000 people. Holyoke ranks fifth with 712 cases per 100,000.
Expanding to county-wide data, the report found that Hampden county overall has a rate of 481 cases per 100,000 people, Hampshire County has 123 cases per 100,000 people, and Franklin County has 154 cases per 100,000 people.
Albert Park is a harm reduction worker and co-founder of HRH413, a community organization that provides harm reduction services for people with substance use disorders across western Massachusetts. He founded it about a year ago alongside co-founder Jess Tilley.
“One of the things we’re trying to do is serve the underserved populations, people who would avoid typical brick and mortar sites because they don’t trust institutions, whatever the reason. We will do street outreach to try to reach those people,” Park said.
He said he finds it alarming that HIV is rising in Massachusetts.
“Things came to [the state’s] attention because of stuff that was happening in eastern Massachusetts, but there’s definitely been a noticeable rise in seroconversion rates [the period of time in which HIV antibodies develop and become detectable] in this area as well,” he added.
As for the cure now being researched, Park argued that if a cure for HIV is found, financial access to that cure would be a major issue.
“Who gets to be cured of HIV?” he said. “It would be wonderful to say that this would be open to everyone and we know that’s absolutely not true just because of access to medical care. Access to medical care is not equitable. We know that. That’s the way things are in this country at this time.”
Park believes that education surrounding HIV prevention needs to be more robust, not only in Massachusetts, but overall.
“I don’t know if that’s a result of people sort of taking their foot off the gas a little bit because of the antiretroviral [drugs] — the fact that there are effective therapies at this point,” Park said. “But people are starting to forget that people still do die of AIDS … This does not have to happen. We already know how to curb it.”
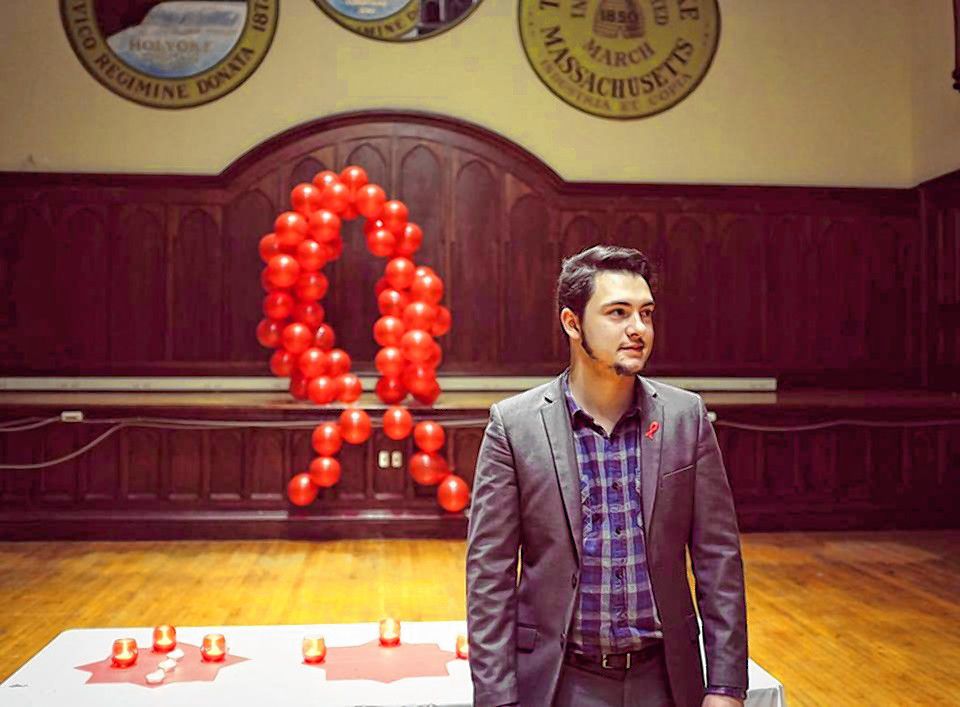
Paulo Salvador, a 23-year-old gay man and Longmeadow resident, contracted HIV when he was 19 years old. His former partner of two years did not disclose that he was HIV positive. Salvador only learned that he was HIV positive from his former partner after going to get tested alongside another partner.
“His came out negative and mine came out positive, so I had less than 15 minutes to figure out how the fuck I was going to tell my partner,” Salvador said. “We’d already been together for a year at this point in time.”
Salvador said his former partner hid the fact that he was also HIV positive for years prior to their relationship, leading Salvador to believe that he may have transmitted HIV to his former partner rather than the other way around.
“Here I am thinking that I gave it to this person,” Salvador explained. “So obviously you’re like, ‘Fuck. Now I just killed someone else.’ And come to find out, this person had been positive for years prior to me even knowing them.”
He said it was a traumatic experience for him when he was diagnosed.
“I felt like I was going to die and felt betrayed,” he said.
Salvador’s only experience with HIV at the time was in regards to this aunt Sherry, who battled AIDS for years, eventually passing away from AIDS-related liver and kidney failure at the age of 47.
He thinks that pushing for education and increased prevention is how HIV/AIDS would be eliminated.
As for a potential cure, Salvador said he was skeptical that low-income people would be able to have access to it.
“Our pills now are fucking $4,000,” Salvador said, adding that while it is covered by insurance, there are other life-saving drugs that are not. “Our country, with the way that our healthcare system is, it’s all about money.”
He said the drugs he takes to manage his HIV also have caused some damage to his liver and kidneys. Salvador is worried about the long-term effects HIV drugs have on his own body and for others who have HIV.
HIV drugs are intended to maintain good health, but the human liver recognizes these drugs as toxic compounds, according to the U.S. Department of Health and Human Services website. Because of the drugs, the liver can become overworked, which can lead to liver damage if drugs are taken over a long period of time.
After seeking treatment, Salvador went on to work with HIV-related organizations. He later founded his own non-profit organization in 2017, Holyoke-based Project LIFE (Live, Inspire, Further, Educate), which provides advocacy, support, and education to the HIV positive community in the Pioneer Valley.
“I wanted to create an organization that would take on all of the burden of the diagnosis and help people live happier, healthier lives,” he said. “We take on a lot of responsibility for the clients like managing doctor appointments. We check to make sure that our clients have food at home because you have to be well nourished in order for the medication to work.
He continued, “We make sure that they’re not homeless and out on the street because that’s another struggle. We basically try to make it so that their life is as normal as possible; take off all of the burden.”
Salvador said that in order to truly eliminate HIV, not only do we need more funding, but everyone should be tested for the virus.
“If you really want to fucking clean this virus out; fucking test people … How are you not going to spread it if you don’t know you have it or not? If you’re not taking preventative measures, then it’s just going and going and going.”
Inside a pink, Queen Anne Victorian-style home in Holyoke called “The Pink Lady” are thousands of books, newspapers, and magazines as well as hundreds of videos and audio recordings chronicling LGBTQIA+ history throughout the world. This building, built in 1885, is the home of the Sexual Minorities Archives, which has been part of the Pioneer Valley since 1979. Originally founded in Chicago, Illinois, the archives moved to Northampton in 1979, then to Holyoke in 2015.

Ben Power Alwin, who is the executive director/curator of the Sexual Minorities Archives in Holyoke, talks about his work in the foyer of the archives, Tuesday, April 23, 2019.
The curator of the Sexual Minorities Archives and homeowner is Ben Power Alwin, a transgender man and queer historian, who told the Valley Advocate about the history of queer culture in the Pioneer Valley, and the troubled history of federal agencies turning a blind eye to the AIDS crisis in the gay community.
He said lesbian women were the first people in the LGBTQIA+ community to start businesses and develop a community in Northampton starting in the 1970s. And when the AIDS crisis hit a decade later, lesbian women often were caregivers to their sick or dying gay male friends who were shunned by their families, Alwin said.
Alwin said he’s skeptical that any potential cure would benefit the majority of people living with HIV. He said that if an HIV cure were discovered, the cost would likely not be affordable to the average person.
“That’s not what happens today with really expensive treatment,” he said. “I say this because I have a different illness that requires chemotherapy every six months. And one chemotherapy infusion is $12,000. I have to have three insurances to cover that.”
Prior to the first Lesbian and Gay Liberation March, which later developed into Noho Pride, Alwin, who attended that 1982 march, said lesbians in the Valley were mostly separate from gay men. The march was started out of a group called Gay and Lesbian Activists, which formed out of the University of Massachussetts Amherst.
But out of the tragedy of the AIDS crisis came a newfound sense of urgency for gay men and lesbians fighting for equal rights and for HIV/AIDS research and treatment options, which locally impacted the early years of Noho Pride.
This was one of the first instances of gay men and lesbians uniting in the Pioneer Valley to fight for equal rights, he said. Although, the march wasn’t in direct response to HIV/AIDS, the AIDS crisis did play a role in bringing lesbians and gay men together.
Today, Noho Pride (which will happen this Saturday) brings more than 40,000 people to downtown Northampton to celebrate the LGBTQIA+ community and straight allies often outnumber gay men, lesbians, transgender men and women, and others in the parade, according to JM Sorrell, a media spokesperson for Noho Pride. As gay men and lesbians gained more rights in Massachusetts, the event became more geared towards fighting for rights and celebrating.
Sorrell said the AIDS crisis didn’t contribute to the formation of the Lesbian and Gay Liberation March in Northampton, but throughout the 1980s and 1990s, the crisis was a driving force for gay men and lesbians fighting for equal rights, not just locally.
“There were fights for lesbian and gay rights before the AIDS crisis,” she said. “I would say the AIDS crisis certainly spoke to the urgency of justice and equality in a very acute manner. Like any social justice or civil rights movement, action comes from crisis and a lack of rights. I would call it a very major force in lesbian and gay liberation.”
Meanwhile, in the 1980s medical community, stereotypes about AIDS often persisted, Alwin said. Doctors wouldn’t touch HIV or AIDS patients due to fears that they would be contaminated.
“So, more often than not, gay men were dying in their own homes, and in a lot of cases their families rejected them. And so, who was going to take care of them? It turned out to be the women a lot of the time.”
Alwin said one of his good friends, the father of the trans male community in San Francisco, Lou Sullivan, died of AIDS in 1990 after living with the illness for six years.
“At the time, he was the only other trans man that I knew,” he explained. “He was my buddy, so I know the pain of [losing someone to AIDS].”
In Northampton during the 1980s, there was a pioneer organization in AIDS prevention in the Valley called the Family Planning Council, which gave out condoms and gave HIV testing. Today, the Family Planning Council goes by another name — Tapestry Health, which continues HIV prevention work through street outreach and education for at-risk communities across Western Massachusetts.
On a federal level at the same time, the AIDS crisis was also mostly ignored by the Ronald Regan presidency, Alwin said.
“They basically said, ‘Let them die.’ They didn’t do anything. They have blood on their hands. All these Americans were dying of AIDS and they did nothing as far as funding programs. It was gay people having to come up with programs like [the Family Planning Council] in Northampton.”
Grassroots organizing raised awareness about the hundreds of thousands of people dying from AIDS. One prominent advocacy group with chapters across the country was the AIDS Coalition to Unleash Power (ACT UP), which organized protests on Wall Street, at schools, and across the United States after it was formed in March 1987. That same year, the first drug to treat HIV — AZT — became available as a treatment option for those with the illness.
Today, there is a drug called pre-exposure prophylaxis (PrEP), also known as Truvada, which is a daily pill that prevents HIV infection and is typically prescribed to those who are HIV negative, but are also at a higher risk of being exposed to the virus via lack of safe sex or injection drug use, according to the Center for Disease Control and Prevention’s website. When taken consistently, the two-medicine drug combination reduces the risk of HIV infection in people by up to 92 percent.
Granowitz, the Northampton doctor, said people are typically being diagnosed with HIV earlier now compared to past decades. However, one enormous hurdle for the disease is called the HIV treatment cascade.
About 86 percent of the 1.2 million people living with HIV are diagnosed, according to HIV. org. But only 40 percent become engaged with care, 37 percent go to receive treatment, and only 30 percent of those people have their HIV virally suppressed.
Alwin sees the relatively new prevention drug (it was approved by the Food and Drug Administration in 2012), as both a positive and negative for HIV patients.
“That is progress for the world, however we’re not there yet. There’s a plus and minus for this whole Truvada thing. One of the minuses is the cost: it’s $2,000 a month or more. Health insurance covers it … However, if you don’t have access to health insurance or if you’re not on Medicaid, you can still get HIV, especially communities that are using needles and are economically impoverished,” Alwin said.
During his state of the union address this year, President Donald Trump announced a new effort “to eliminate the HIV epidemic in the United States with 10 years.” However, it’s well documented that Trump has gone back on his word many times on several different issues, and HIV treatment advocates are tempering their optimism that his administration will take the needed steps to end the crisis.
According to Trump’s proposed fiscal year 2020 budget, $291 million is being requested for the initiative to end HIV/AIDs.
But according to the Joint United Nations Programme on HIV/AIDS, in order to end AIDS as a public health threat by 2030, it’s estimated that $26.1 billion would be required for the global HIV response in 2020 alone.
Shally-Jensen said she thinks 10 years isn’t a realistic time frame for eliminating the disease.
“How’s he going to eliminate it?” she asked. “We’ve all been trying to eliminate it since it started; since we realized what it was. You always need more funding for everything in order to make that happen.”
As an infectious disease doctor, Granowitz said he isn’t sure if the target goal to eliminate HIV is practical, but is glad that ending HIV/AIDS is a topic that’s being discussed.
“I don’t know if we’ll be able to do that, but it’s an awesome goal,” he said.
Alwin, curator of the Sexual Minorities Archives, said HIV drugs today are managing the illness, but not wiping it out. He argued that there needs to be more funds allocated for HIV and AIDS research.
“The United States government owes an amends now [because of Reagan’s administration] and should be stepping up funding for AIDS prevention and a cure … But, no. That’s not the government we have in power now,” he said.
Chris Goudreau can be reached at cgoudreau@valleyadvocate.com.